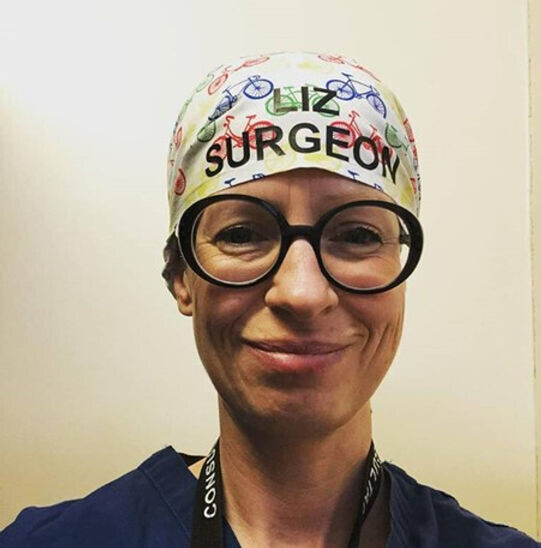
Dr Liz O’Riordan: "I’m a breast cancer surgeon – this is what surviving cancer myself taught me" Daily Telegraph UK
By Rosamund Dean
As a breast surgeon, Dr Liz O’Riordan is well acquainted with worst-case scenarios. So, when she discovered a lump on her breast in 2010, her initial reaction was terror. “I remember howling on the sofa: ‘I’ll be dead in a year,’” she says. “I thought it was the end of the world.” To her relief, the lump was a benign cyst. In 2014, she noticed another lump. Calmly this time, she went for a scan and, again, it was a cyst. Early 2015, the same story: another lump, another cyst.
When a further lump appeared six months later, she almost didn’t go back, but her mum insisted. “I looked up at the screen during the ultrasound and saw a cancer,” she remembers. This was at the Suffolk hospital where she had trained and been based for three years – and where her husband Dermot, a general surgeon, worked. So, the diagnosis was a blow not only for Dr O’Riordan and her husband, who was in the room to receive the biopsy results, but also for the surgical staff on the oncology team, who were like family. “When I got the results of the biopsy, everyone was crying,” she says. “My consultant was crying; my husband was crying. But I felt like I was looking down on someone else. Like, it can’t be real.”
O’Riordan during her treatment for breast cancer. Photo / Instagram
Unlike her frenzied reaction to the first lump five years earlier, she remained calm and practical, calling her parents in Scotland to explain her diagnosis and treatment. “You sound like you’re talking about a patient instead of yourself,” her mum noted.
She was lucky to have been diagnosed in time for treatment to be curative, but, since she was only 40, she’d receive the works: chemotherapy, mastectomy surgery, radiotherapy, and hormone therapy.
Her insider knowledge was both a blessing and a curse. “I wanted to tell my surgeon: ‘Can you use this stitch, and put the drain here,’” she laughs wryly. “And she had to say: ‘Stop. You need to be a patient.’ But I was more aware of the things that can go wrong.”
Dr Liz O’Riordan was diagnosed with breast cancer in 2015. Photo / Instagram
Although an expert on the surgical side, Dr O’Riordan was shocked to learn how little she knew about the psychological impact of breast cancer treatment, particularly when thrust into a brutally abrupt menopause caused by hormone therapy. She would tell patients that symptoms would last around six months, “because that’s what I’d heard. I had no idea what it was like.”
“Going into instant menopause at 40 was the hardest thing, and a massive learning curve,” she says now. Some menopausal symptoms can improve after six months, but others are more permanent and a vast array – from brain fog and headaches to insomnia and joint pain – are not yet fully understood or treated.
O’Riordan says she was shocked to learn how little she knew about the psychological impact of breast cancer treatment. Photo / Instagram
“I knew nothing about the impact it would have on my relationship, with night sweats meaning no spooning in bed. We had to find new ways of being intimate and deal with the depression and anxiety.
The stress that cancer puts on a relationship is so hard, when you don’t feel sexy, you don’t like how you look and you don’t want anyone to touch you. It takes time to learn to like yourself again before you can let your partner like you.
Dermot and I have always been really open with each other. We talk about everything and he understands – he’s great at listening. I’m very lucky to have that, because I know a lot of women get divorced when this hits them; it’s too much for their partner to cope with.”
Although happily child-free pre-diagnosis, having the option of motherhood taken away from her was extremely distressing. At her lowest ebb, she told Dermot to leave. “I felt guilty,” she explains. “He didn’t sign up for this. I said: ‘Go and find a woman with healthy breasts and a libido to match.’ I wouldn’t let him look at me because I was embarrassed of the scars.”
O'Riordan says she wants to help more women feel confident after mastectomy surgery. Photo / Instagram
Having spent years performing complex surgeries, suddenly brain fog meant she couldn’t remember the word for a pen. She realised that many post-treatment issues are invisible.
Your hair might have grown back, but you may still be struggling. “You smile and you put on a face, and everyone says you look great,” she says. “But there’s so much going on, including fear of recurrence.” If breast cancer returns and spreads – usually to the bones, brain, liver, or lung – then it is no longer curable, and the fear of this happening can be all-encompassing.
In 2018, Dr O’Riordan had a local recurrence in her chest wall, which is when the cancer returns but is caught before metastasising elsewhere in the body. This exacerbated the anxiety she was already feeling.
“It reached a point where I was almost wanting my cancer to come back so that I can stop waiting for it to happen,” she explains. “Obviously I don’t want to have stage 4 cancer, but I had no idea that the roller-coaster of depression, anxiety and fear would be with me for the rest of my life.”
While the fear never completely goes away, she eventually found a way to stop it from controlling her life. “I can reduce the risk of it coming back by exercising, not really drinking and eating well, but I’ve accepted it’s out of my control,” she says. “So instead of worrying about the odds, I just have to live my life.” How long did it take to get to that place? “Five years.”
Surgery itself was also a shock. Having initially had reconstruction with an implant, radiotherapy had caused it to go “hard and tight, like a tennis ball”. She had it removed and is now flat on one side. “I remember walking around Debenhams in floods of tears because they didn’t have mastectomy bras in my size,” she says. “I thought, what am I going to do? I’m going to be a hunchback for the rest of my life so no one sees me lopsided. I thought my life, in terms of going out socially, was over.”
Although she says she has now come to terms with her post-mastectomy body, it’s almost like a sense of grief that’s always there, with good days and bad days. At one point she admits “it’s still hard to look in the mirror”, but then continues: “I’m lucky that I’m small-breasted, so it’s not that obvious. I’m not ashamed anymore. And I want to empower women to be confident after mastectomy surgery.”